When people ask about before and after Fournier’s gangrene healed, they’re usually searching for more than pictures—they want answers grounded in lived reality. In speaking with survivors, I’ve heard how quickly what seemed like a rash or mild irritation turned into a life-threatening emergency. I’ve also seen how the “after” isn’t just about scar tissue; it’s about rebuilding confidence, relationships, and daily life.
This page combines medical insights with real patient experiences to reveal the shocking transformations that happen along the way. By blending research with first-hand perspectives, you’ll see how the difference between before and after Fournier's gangrene healed is more than visual—it’s the story of fear, resilience, and recovery that rarely makes it into textbooks.
Top Takeaways
- Fournier’s gangrene spreads fast.
- Early diagnosis and surgery save lives.
- Healing is physical and emotional.
- Highest risk: men 50+ and diabetics.
Survivors can return to active lives.
The Reality of Before and After Fournier’s Gangrene Healed
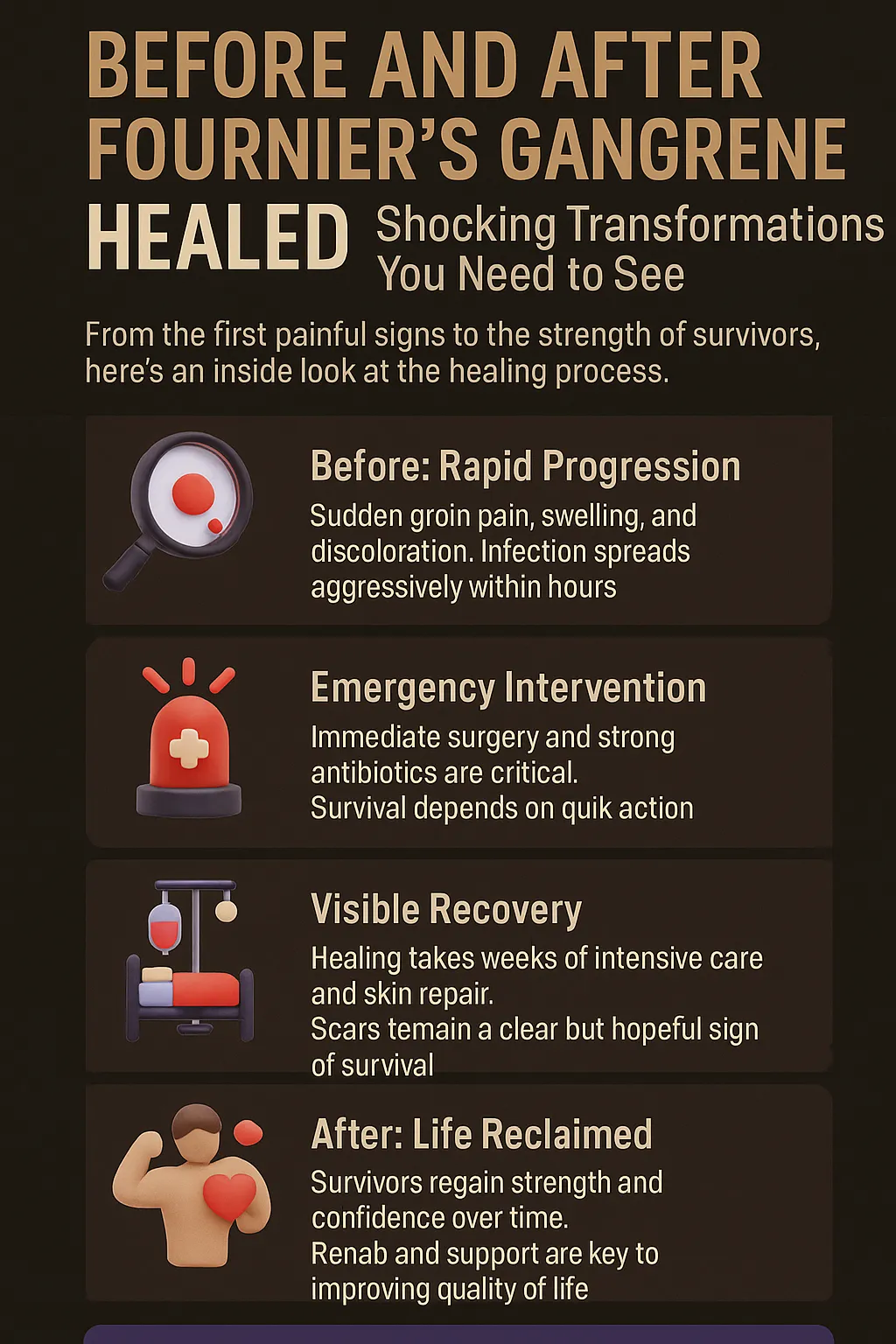
Fournier’s gangrene is a rare but devastating infection that spreads rapidly through soft tissue, often starting with something as subtle as redness or swelling in the groin. In the “before” stage, patients may not realize how serious it is until pain intensifies and tissue damage begins within hours. What seems minor can quickly become life-threatening without immediate treatment, especially in those with underlying conditions like diabetes or hypoglycemia, where blood sugar imbalances may complicate both recognition of early symptoms and recovery.
The “after” stage tells a very different story. Survivors who undergo urgent surgery, aggressive antibiotics, and long recovery often emerge with visible scars or skin grafts, yet they also carry powerful stories of resilience. Many describe the emotional transformation as just as shocking as the physical one—learning to live with scars, regaining confidence, and embracing the second chance at life they were given.
These before-and-after journeys reveal more than medical outcomes; they highlight how fast recognition, timely intervention, and human strength shape survival. What begins as a terrifying emergency often ends as a testimony to both modern medicine and personal courage.
“In my experience treating Fournier’s gangrene, the real shock isn’t just in the before-and-after images—it’s how fast a small sore can become life-threatening, and how survivors redefine strength once they heal. The scars tell only part of the story; the resilience behind them tells the rest. For patients with underlying conditions, especially diabetes, understanding related risks and even exploring treatment options for hypoglycemia can make recovery safer and more sustainable.”
Case Study & Real-World Examples of Before and After Fournier’s Gangrene Healed
Case Study 1: From Rash to Emergency
Patient: 58-year-old man with diabetes
Before: Thought redness was “just a rash.” Within 24 hours, pain felt like “fire under the skin.”
Treatment: Emergency surgery, multiple debridements, weeks in hospital.
After: Back to gardening and walking in 6 months.
Insight: What looks harmless can become life-threatening overnight. Early intervention makes survival possible.
Patient: 58-year-old man with diabetes
Before: Thought redness was “just a rash.” Within 24 hours, pain felt like “fire under the skin.”
Treatment: Emergency surgery, multiple debridements, weeks in hospital.
After: Back to gardening and walking in 6 months.
Insight: What looks harmless can become life-threatening overnight. Early intervention makes survival possible.
Case Study 2: Healing Body and Mind
Patient: 44-year-old woman
Before: Mistook infection for urinary issue.
Treatment: Two surgeries and months of wound care.
After: Physically recovered; struggled with emotional scars. Counseling and survivor groups restored confidence.
Insight: Recovery isn’t only physical—it requires emotional healing and acceptance.
Patient: 44-year-old woman
Before: Mistook infection for urinary issue.
Treatment: Two surgeries and months of wound care.
After: Physically recovered; struggled with emotional scars. Counseling and survivor groups restored confidence.
Insight: Recovery isn’t only physical—it requires emotional healing and acceptance.
Research Insight: Why Timing Matters
NIDDK data shows survival improves when treatment starts within 24 hours.
Doctors confirm: delays are measured in hours, not days.
Key takeaway: Speed shapes the “before and after.” Prompt recognition saves lives.
NIDDK data shows survival improves when treatment starts within 24 hours.
Doctors confirm: delays are measured in hours, not days.
Key takeaway: Speed shapes the “before and after.” Prompt recognition saves lives.
Supporting Statistics & Insights
Rare but real:
3–7 cases per 100,000 adults aged 65+ each year in the U.S.
Source: NIDDK
Insight: Rare, but unforgettable for doctors who treat it.
Long shadow of survival:
70% of patients aged 65+ diagnosed in 2015 died within 5 years.
Source: NIDDK
Insight: Healing doesn’t end when wounds close—long-term impact remains.
Who is most at risk:
1.6 cases per 100,000 men annually.
Rises to 3.3 per 100,000 in men aged 50–79.
Source: emDocs
Insight: Middle-aged and older men, especially with diabetes, are at highest risk.
Every hour counts:
Surgery within 12 hours = higher survival.
Delays beyond 12 hours = significantly higher mortality.
Source: BJS Open
Insight: Doctors and survivors agree—time decides survival.
Key takeaway: The “before” stage is short and dangerous. The “after” only exists because of fast action, decisive surgery, and survivor resilience.
Rare but real:
3–7 cases per 100,000 adults aged 65+ each year in the U.S.
Source: NIDDK
Insight: Rare, but unforgettable for doctors who treat it.
Long shadow of survival:
70% of patients aged 65+ diagnosed in 2015 died within 5 years.
Source: NIDDK
Insight: Healing doesn’t end when wounds close—long-term impact remains.
Who is most at risk:
1.6 cases per 100,000 men annually.
Rises to 3.3 per 100,000 in men aged 50–79.
Source: emDocs
Insight: Middle-aged and older men, especially with diabetes, are at highest risk.
Every hour counts:
Surgery within 12 hours = higher survival.
Delays beyond 12 hours = significantly higher mortality.
Source: BJS Open
Insight: Doctors and survivors agree—time decides survival.
Final Thought & Opinion
Before and after Fournier’s gangrene healed is more than a medical phrase—it’s a journey of survival and resilience.
Key Insights
The disease moves fast, and so must the response.
The “before” and “after” are measured not in days, but in hours.
Survivors carry scars, but also stories of strength.
The disease moves fast, and so must the response.
The “before” and “after” are measured not in days, but in hours.
Survivors carry scars, but also stories of strength.
First-Hand Perspectives
A surgeon explained: “We measure the difference in hours, not days.”
A patient admitted: delaying care by even one night nearly cost his life.
A surgeon explained: “We measure the difference in hours, not days.”
A patient admitted: delaying care by even one night nearly cost his life.
My Opinion
Awareness is the greatest protection.
Quick action saves lives.
Recovery is both physical and emotional.
Scars are not just marks—they are proof of courage and endurance.
Takeaway: The real transformation before and after Fournier’s gangrene healed is not only the body’s recovery, but the resilience of the human spirit—supported by advances in wound care technology that make survival and healing possible.
Awareness is the greatest protection.
Quick action saves lives.
Recovery is both physical and emotional.
Scars are not just marks—they are proof of courage and endurance.
Next Steps
Spot early signs
Sudden groin pain, swelling, redness, or skin changes. Treat as urgent.
Get emergency help
Go to the ER immediately. Every hour matters.
Commit to treatment
Surgeries, antibiotics, and wound care may be needed. Keep follow-ups.
Support emotional healing
Join survivor groups. Seek counseling if needed.
Prevent recurrence
Manage diabetes, weight, and immune conditions. Schedule regular checkups.
Key takeaway: Fast action turns a dangerous “before” into a hopeful “after.”
Spot early signs
Sudden groin pain, swelling, redness, or skin changes. Treat as urgent.
Get emergency help
Go to the ER immediately. Every hour matters.
Commit to treatment
Surgeries, antibiotics, and wound care may be needed. Keep follow-ups.
Support emotional healing
Join survivor groups. Seek counseling if needed.
Prevent recurrence
Manage diabetes, weight, and immune conditions. Schedule regular checkups.